A young woman sits on the couch in Dr Amy Abernethy’s clinic at the Duke University Medical Centre. The woman, who is in her thirties, has just been told that the same type of cancer that had claimed her mother’s life was spreading in her; that she, too, had a type of aggressive skin cancer, called melanoma. The only thought she can grasp, among the many questions sumeraulting through her mind is: Can I still have a baby?
All that Abernethy wanted to say is: Yes, absolutely. And set up a treatment plan that would not only curb the cancer but make having a family possible for her patient. After all, Abernethy’s clinic is sandwiched between research laboratories racing to develop new and better treatments for patients like hers. But it was the early 2000s, and the reality for patients with advanced melanoma at that time was grim. The road for new treatments from bench-to-bedside was slow and circuitous.
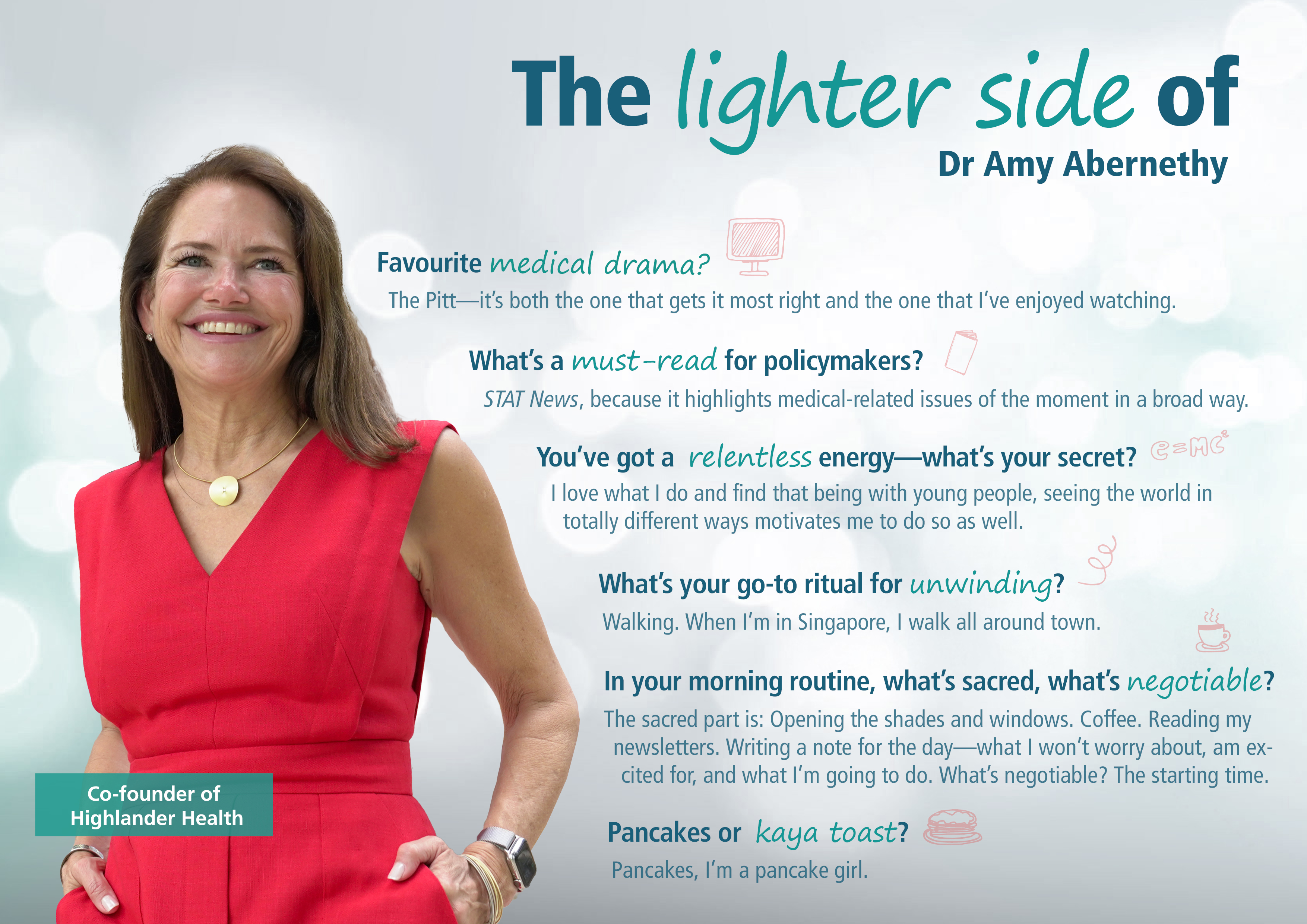
That experience lit a fire in Abernethy—a North Star that would guide her career, as she seeks to transform the road of clinical research into safe, but fast-flowing highways, so that effective and safe treatments can reach patients faster. In pursuit of this mission, she co-founded the Centre for Learning Healthcare at Duke, joined healthcare technology startups, co-founded her own startup Highlander Health, and even completed a stint at the US Food & Drug Administration, where she worked as principal deputy commissioner.
Here, Nicole Lim catches up with Abernethy to find out how she’s progressing on her quest.
MEDICUS: Thank you, Amy, for joining us. I wanted to start by asking you if there was a personal “light bulb” moment that moved you from being an academic and oncologist to a data-driven entrepreneur and “reformer”?
Amy Abernethy: So I’ve been motivated by the same question my entire professional career: How do we get treatments that work to the people who need them as quickly as possible. When I was an academic at Duke, I was working on how to leverage data and technology to more quickly conduct clinical research. But I was limited by two things:
- Access to engineering, because if we’re going to leverage data and technology, then we really needed to be able to deploy software engineering.
- And just the scale of capital required, because typically technology development requires software engineering and investment at scale that is different from traditional academic grants.
I realised if we’re going to solve this problem, then maybe I needed to go to the places where those things were the norm. As a result, my professional career has been studying things in academia, figuring out a legitimate path forward to make the discovery highways faster, then going to industry to build the capabilities, then going to regulatory to make sure that the rules are clear enough that anybody can move down those highways, and going back and forth again ever since.
MEDICUS: What’s the single most urgent issue in healthcare that your company, Highlander Health, was built to solve—and why that one?
Amy Abernethy: All the investments in biology over the last century have led to remarkable innovations. But now the choke point is getting them through our evaluation pipeline, which is clinical research, so we can get them to patients. I co-founded Highlander Health with my longtime colleageue and fellow Duke alumni, Brad Hirsch, to solve some of these challenges.
And that’s what Highlander Health is singularly focused on: Accelerating the path of clinical research, clinical evidence generation to get treatments that work to the people who need them as quickly as possible, and to smooth the path towards personalised healthcare.
Highlander Health is an investment firm with two parts. The first is the Highlander Health Institute, where we’re building a public interest platform by giving non-profit grants to health systems and others to test ideas that have been talked about for a long time. So there’s no intellectual property gained, no goals towards return on investment beyond societal return on investment.
For example, we’ve given a grant to the Baylor, Scott & White Research Institute to look at what it takes to be able to use data that exists in a health system, in the electronic health records, echocardiography systems and other electronic databases, to fill in the case report forms of federally mandated databases needed to meet FDA requirements or payer requirements. And not only do we want to work together with Baylor, Scott & White to figure out how to connect these disparate systems, but we want to document that and then test it out in the next health system. So that we can figure out what it takes to transfer lessons learned.
The second part is Highlander Health Partners, through which we invest in companies that we think are part of a modern evidence generation platform, to invest in and produce successful companies. One difference in our investing thesis is that we either buy the company or take a controlling stake because we want to make sure that we’re investing the capital, knowledge and essentially, elbow grease to help move those companies in that direction.
For example, we acquired a company called Target RWE in January 2025. This is a data company that builds retrospective, longitudinal datasets for liver disease, gastroenterology and dermatology. As well as the existing data, we see an opportunity for Target RWE to collect new data from the same health systems, clinicians and patients, that then form the foundation of prospective and retrospective research blended together as a modern approach to clinical research.
MEDICUS: To achieve your mission of accelerating evidence generation, how do you foresee evidence generation evolving?
Amy Abernethy: Evidence generation will consist of four foundational components: Traditional, prospective clinical trials; retrospective evaluation of data that already exists; combining prospective and retrospective activities; and leveraging data that already exists to complete clinical trial datasets to reduce the documentation burden and make any kind of clinical research more efficient.
With this platform, you can layer on lots of different things. You can layer on modern study designs, such as novel randomisation approaches like five-to-one randomisation where the control arm is partially prospectively collected and partially retrospectively completed or simulated. You might layer in human challenge studies or different exposures to understand longitudinal safety, beyond the clinical trial. All of this now becomes way more doable.
And that, in turn, sets us up to deliver personalised healthcare, which will require more detailed information that is specifically helpful to you. For example, I use a sensor on my finger to understand how I sleep, how much I exercise, and hopefully soon, to understand my blood sugar, and use that to adapt every single day what my exercise plan should be, what I should eat, what time I should go to bed.
So part of what we’re trying to build towards at Highlander Health are the kind of data platforms that make those datasets available, and much more easily accessible, to enable those personalised healthcare adjustments.
MEDICUS: To achieve your mission of accelerating evidence generation, how do you foresee evidence generation evolving?
Amy Abernethy: Evidence generation will consist of four foundational components: Traditional, prospective clinical trials; retrospective evaluation of data that already exists; combining prospective and retrospective activities; and leveraging data that already exists to complete clinical trial datasets to reduce the documentation burden and make any kind of clinical research more efficient.
With this platform, you can layer on lots of different things. You can layer on modern study designs, such as novel randomisation approaches like five-to-one randomisation where the control arm is partially prospectively collected and partially retrospectively completed or simulated. You might layer in human challenge studies or different exposures to understand longitudinal safety, beyond the clinical trial. All of this now becomes way more doable.
And that, in turn, sets us up to deliver personalised healthcare, which will require more detailed information that is specifically helpful to you. For example, I use a sensor on my finger to understand how I sleep, how much I exercise, and hopefully soon, to understand my blood sugar, and use that to adapt every single day what my exercise plan should be, what I should eat, what time I should go to bed.
So part of what we’re trying to build towards at Highlander Health are the kind of data platforms that make those datasets available, and much more easily accessible, to enable those personalised healthcare adjustments.
“There is a lot of magical thinking assigned to AI that doesn’t give voice to the fact that we still have to develop the solutions, test that they work, figure out how to deploy them, and figure out implementation.”
MEDICUS: You’ve worked across the healthcare spectrum—from care delivery to innovation, regulation, and beyond. Where, and what, are the biggest breakdowns in the system that still frustrate you?
Amy Abernethy: Hands down, the biggest breakdown in the system is that we are too caught up in the cost of things. So we remove access to things because we’re worried about the cost. For example, limiting the number of physical therapy visits due to cost rather than need, or starting with the cheapest medicine rather than the best medicine. That’s the problem to solve. If we can get smarter about delivering the right treatment to the person who needs it, not because of cost avoidance, but because that’s the correct thing to do; and if we can get smarter about abundance in healthcare and not scarcity, every one of us would experience healthcare in a more positive way.
MEDICUS: How will the success of Highlander Health impact clinical evidence generation?
Amy Abernethy: At Highlander Health, our goal is to reduce the timelines for clinical trials and clinical research by 50 per cent or more. That’s our 10-year-plus vision. I also believe that the foundational datasets and capabilities, and methods we’re going to need to get towards that Highlander Health vision set us up for the kinds of data that allow us to hit the next horizon, which are all the personalised healthcare adjustments.
MEDICUS: AI is reshaping healthcare faster than many imagined—what’s underrated and what’s being overhyped?
Amy Abernethy: What’s being overhyped about artificial intelligence (AI) is what I call the “blinking light” problem. This thinking that it’s all sitting right below the surface, and we just haven’t turned it on in the right way yet. I feel like there is a lot of magical thinking assigned to AI that doesn’t give voice to the fact that we still have to develop the solutions, test that they work, figure out how to deploy them, and figure out implementation.
On the under-appreciated side is the fact that there is going to be, and there already are, a massive number of solutions that are going to start working together to continuously help and support us, and that we need to do the detailed work to develop each one. That detailed work is important, and frankly, we don’t have enough people deployed against it. We will have so many AI capabilities that could be brought to bear on health where the system is just gummed up, not ready to figure out what solution we need, how to adapt it for a local scenario, deploy it for patients, and monitor it. We just haven’t done all of that work.
MEDICUS: As a Duke trustee, where/how do you see Duke shaping the future of health and medicine?
Amy Abernethy: Duke provides innovation, creativity, access to the right kinds of scientific and engineering talent, and the forward-looking vision that provides the inquiry needed, including for a longer-term horizon. When you’re building companies, the horizons you’re building for are short, whereas when you’re an academic health system, you can imagine a world 20 or even 100 years from now, and figure out how to explore and get creative and project into that environment. So that is part of the reason I came back, because I think that the academic health system now and into the future has that core responsibility, and Duke is uniquely set up for that.
MEDICUS: Looking back, which bold decision most altered your career trajectory?
Amy Abernethy: Oh, easy: Saying “Yes, let’s see how we can make it work” in response to my husband’s announcement late one Friday night that he had just been offered his dream job in Australia, even though initially I couldn’t imagine what I was going to do. In the United States, I had gone to medical school, I was chief resident of medicine and becoming an oncologist, and suddenly he’s telling me that he’s just been offered the job of a lifetime in another country. After having supported me through medical school and moving to North Carolina, what could I say? So, I started talking to mentors all over Duke to work out how to do it.
I ended up writing and getting a grant from the US National Cancer Institute. I moved to Australia, worked with the chair of medicine at Flinders University in South Australia, got a PhD, and had two children. I learnt how to run clinical trials and work in a completely different healthcare system. I learnt about palliative medicine and about living in a different part of the world. And throughout, I worked for Duke, and continued to cultivate this incredibly meaningful relationship.
MEDICUS: Having made that bold decision, what advice would you give someone looking to launch a healthcare start-up today, beyond ‘solve a real problem’?
Amy Abernethy: For someone who comes from medicine or any other career that has required long-term personal investment, I have three pieces of advice:
- Understand the problem that you’re trying to solve. It may be scratching an itch right in your personal creativity and curiosity, but understand why you’re doing it.
- Mitigate some of the risk. So, if you’re a clinician, can you keep one foot in medicine by seeing patients a day or two a week, so that you stay up-to-date in medicine? Or does it mean that you maintain a research affiliation? Think about ways to mitigate the risk so that all of the investment that you’ve made up until that point is still able to support you into the future.
- Do a bit of signal finding before you make the jump. Talk to many different people and look for a consistent signal that says this is what you should do. And then make the jump. And once you’ve jumped, be all in.